By Sarah Penney, a U of G student writer with SPARK (Students Promoting Awareness of Research Knowledge)
Wear and tear from repetitive use or joint injury is thought to be a major cause of osteoarthritis, an affliction that plagues one in 10 Canadians. New research by Prof. John Srbely and graduate student Gaayathiri Jegatheeswaran in the Department of Human Health and Nutritional Sciences may provide insight into the mechanisms of joint dysfunction associated with osteoarthritis and other degenerative joint diseases.
They say the key is something called “central sensitization.” It’s the scientific term for heightened nerve sensitivity seen in individuals suffering with osteoarthritis. Srbely and his team believe that central sensitization may lead to changes in muscle function as well as promote inflammation.
“Identifying and addressing changes in nerve excitability in the early stages of the osteoarthritic disease process may help to significantly slow the progression of osteoarthritis,” says Srbely.
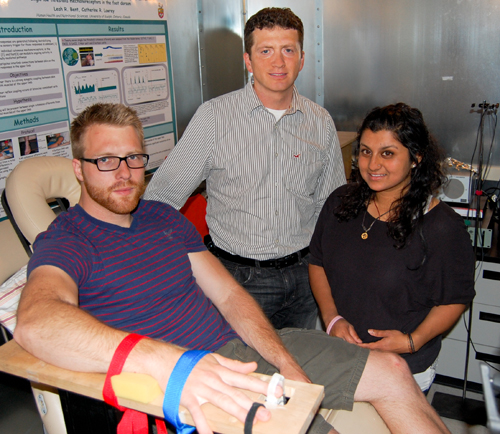
He led a study that compared nerve excitability in the muscles of people with osteoarthritis to others not suffering from the condition. The researchers did this by applying a sensitizing cream to the skin of participants and subsequently measuring muscle activity with a technique called electromyography.
The cream was used to temporarily excite the nerves in the spinal cord and produce a state of central sensitization. The researchers wanted to see whether the muscles of osteoarthritic subjects would respond differently from those without osteoarthritis.
Srbely and his team found that, after applying the cream, the muscles of both groups were more excitable. However, the osteoarthritic group showed significantly more activity. Furthermore, muscle activity in the normal population reduced back to baseline levels after 30 minutes, whereas the osteoarthritic group continued to demonstrate muscle activity well above baseline levels.
This suggests patients with osteoarthritis may have lost the ability to regulate co-ordinated muscle control, which may contribute to joint dysfunction and advance the osteoarthritic process.
Because this lack of muscle control may be active in the early pain-free stages of joint degeneration, Srbely emphasizes that it is important for clinicians to spot these issues early to help patients maintain the best possible joint function and slow down the arthritic process in its early stages.
Srbely says that his team’s findings may contribute to a better understanding of the mechanisms behind osteoarthritis and provide new options for treatment and prevention. This is especially important considering the significant financial burden of musculoskeletal pain on the health-care system, with costs expected to double in the next 30 years due to our aging society.
“Prevention of chronic disease, such as osteoarthritis, will contribute to the sustainability of our health system in the future, and research focusing on the underlying causes and mechanisms of pathology are foundational to this approach,” he adds.
This two-year study was supported in part by the Canadian Arthritis Network.