A first-ever U of G study has proven that opening up tumour blood vessels is potentially more effective in fighting ovarian cancer than destroying the tumour’s blood supply.
Open vessels provide a clear pathway for treatment to attack the tumour, said Prof. Jim Petrik, lead author of the groundbreaking study.
“There hasn’t been much hope for women with ovarian cancer,” said Petrik. “What we are working on has never been done before, and it has the potential to make a significant impact on effective treatment.”
Published recently in the journal Clinical Cancer Research, the study is the first to investigate the impact of establishing a healthy blood supply to a tumour before treatment in mouse models with advanced ovarian cancer.
Current treatment has focused on destroying all the blood vessels and starving the tumour, but it has had poor success, said Petrik.
“When you cut off a tumour’s blood supply, it often becomes more aggressive,” he said. “We developed an approach where you only kill off the dysfunctional blood vessels. The result is a smaller, calmer tumour with a good blood supply. Once you have established an effective vascular system, you can use that system to get treatment to the tumour.”
The researchers worked with mouse models with advanced ovarian cancer because this type of cancer often goes undetected until late stages when survival is low. The current mortality rate for ovarian cancer is 80 per cent.
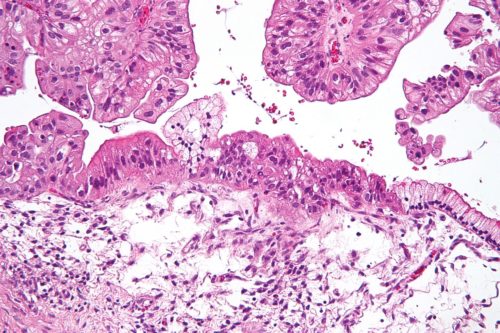
The first step was to prune the blood vessels supplying the tumour. Rapid tumour growth results in a vast, yet dysfunctional, blood supply. After a smaller, healthier blood supply to the tumour was created, the mice were treated with an oncolytic virus. This novel treatment uses viruses to infect and kill cancer cells and to stimulate anti-tumour responses in the body.
“Using an oncolytic virus to treat ovarian cancer is currently under way in human clinical trials, but the success rate is very low. It’s difficult to get the virus to the tumour because of its dysfunctional vascular system.”

By pruning the vessels to create a normal blood supply to the tumour, Petrik was able to dramatically increase the uptake and activity of the virus.
“Using this combination of treatment, we saw the tumour regress from an advanced state, but even more importantly we eradicated the spread of the cancer cells. With this type of cancer, the tumour will grow in the ovary to a large size and then typically spread to the abdomen, causing perforation of the gut or sepsis. Women die from the metastatic nature of the disease, not from the tumour.”
Targeting the tumour’s blood supply and improving it rather than destroying it could also help other treatments, including chemotherapy, that are delivered through the vascular system, he added.
“The treatment for ovarian cancer hasn’t really progressed in four decades. There are limited therapeutic advances, but these findings show that we may be able to improve the effectiveness of our current treatments if we improve the delivery system.”
Contact
Prof. Jim Petrik
jpetrik@uoguelph.ca