
This article is republished from The Conversation under a Creative Commons licence. Read the original article.
COVID-19 vaccines are on the horizon. Lately, it seems like each week brings news of another clinical trial demonstrating vaccine efficacy. But if supplies are initially limited, decision-makers will need to make hard choices about who should get them first.
One approach is to prioritize groups who are most vulnerable to serious outcomes like hospitalization and death, such as the elderly. Another approach is to prioritize groups who are most responsible for spreading the infection. The question is which approach will work best in a given population.
Our team decided to study this question using our combined 30 years of experience in population modelling, including the 2003-04 SARS outbreaks and the 2009 H1N1 pandemic. We developed a mathematical model of COVID-19 transmission and vaccination in Ontario, published as a preprint (a manuscript yet to be checked for errors). The types of models we employ are not mere mathematical abstractions or theories, but rather have been validated for many similar respiratory infections over the past three decades.
We found that if vaccination starts sufficiently early in 2021, a strategy of vaccinating individuals 60 years of age and older will prevent the most deaths. But more surprisingly, we found that if the vaccine is not available until later in 2021, we might be able to prevent more deaths by first vaccinating younger age groups — working-age adults and children — who have more contacts with others.
Vaccines can protect the unvaccinated

To understand this result, we must first explain that vaccines work in two ways. First, they provide direct protection: the vaccinated person doesn’t get infected. Second, they also provide indirect protection: the vaccinated person does not pass infection on to others. We do not yet know if the COVID-19 vaccines will prevent the passing of infection to others, but such transmission-blocking effects are a common feature of most licensed vaccines.
If enough people are vaccinated, the level of indirect protection in a population can be high. And indirect protection can be very powerful. Had it not been for indirect protection, smallpox would never have been globally eradicated in 1977. Once a sufficient number of individuals are vaccinated, herd immunity is achieved. But it is achieved through a kinder, gentler means than letting everyone become infected, and the virus is thereby eliminated from the population. Hence, indirect protection can have very strong effects in real populations.
This is not just the prediction of a mathematical model. This effect has been observed in empirical data on influenza vaccination from Japan, where vaccination of schoolchildren was found to reduce deaths in the elderly. Similarly, some jurisdictions practice cocooning, where if a vaccine does not work in a vulnerable person due to their advanced age or an immature immune system, we vaccinate the people around them instead. This approach is also recommended for the COVID-19 vaccines.
Conditions will change later in the pandemic
We think the switch in strategy between early and late 2021 predicted by our model occurs because indirect protection from vaccines will become stronger, later on in the pandemic.
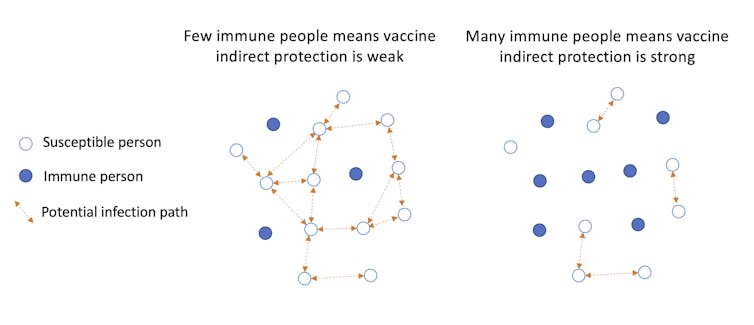
In the early stages of a pandemic, most people are still susceptible. Therefore, if a few individuals are immune because of the vaccine, they don’t protect their contacts since there are too many other ways their contacts could get infected, as illustrated on the left side of the diagram.
However, as time goes on, more individuals will become infected and gain immunity. Under these conditions, adding more immune individuals to the population by vaccination can work more effectively to protect their contacts, as seen on the right side of the diagram. In other words, chains of transmission are replaced by chains of protection. At some point, more deaths can be prevented through indirect protection instead of direct protection.
How to apply this approach
Our model was designed to provide insight into how vaccines work, and not to comment on specific policy recommendations. There are also important caveats to our study. For instance, we did not study a strategy of prioritizing residents of long-term care facilities, most of whom are older than 60 years of age. We also assumed that COVID-19 immunity is long-lasting, although evidence on this is still accumulating. However, the effect we identify relies upon well-validated principles of infectious disease epidemiology, and we found the effect persisted under the various scenarios explored by our modelling.
To apply these ideas in practice, public health authorities would first need to assess population immunity through a survey that tests population blood samples for COVID-19 antibodies a few months before vaccination starts. They could then plug these numbers into a mathematical model to determine whether they should prioritize the elderly, or instead prioritize groups that spread the infection the most.
We think this approach could be feasible. Standard mathematical modelling frameworks could be used, and their predictions are more reliable when predicting months ahead instead of an entire year. Also, antibody surveys are a more accurate way to determine a population’s infection history than case notifications, which would make the model predictions less subject to uncertainties.
Ethical dimensions, and looking to the future
Some might argue that the clear ethical choice is to give the vaccine first to those who are most vulnerable to fatality from the disease. We argue that decisions should be based on best available evidence and consider both direct and indirect effects. If the evidence suggests we can prevent more deaths in the elderly by vaccinating other age groups first, then that is the ethical decision. In other words, the right thing to do requires careful and sometimes nuanced thinking, but always evidence.
Indirect protection may seem like an abstract concept in the grip of a fast-moving pandemic. However, looking ahead , and with hope, we think it will be practically impossible to globally eradicate COVID-19 without it, just as in the case of smallpox. Vaccination policies will have to take advantage of indirect protection sooner or later, in one context or another.
By Prof. Madhur Anand, director of Global Ecological Change & Sustainability Laboratory; Prof. Chris Bauch and Peter C. Jentsch, PhD candidate, applied mathematics, University of Waterloo